While indigestion is common for many Americans, particularly given the standard American diet, if you’re having burning sensations in or above your stomach, stomachaches or pains, feeling nauseous or vomiting, or constantly burping, you may be suffering from gastritis symptoms — and that means you may want to begin the gastritis diet treatment plan.
What is gastritis? It’s a digestive condition caused by damage and inflammation to gastric mucosa, the lining of the stomach and gastrointestinal tract. Erosion of the stomach lining leads to acid causing burning sensations and pain in the digestive system — and sometimes malabsorption of nutrients. Many of the symptoms of gastritis are similar to symptoms caused by stomach ulcers, although gastritis tends to only affect the stomach (as opposed to ulcers, which can also damage parts of the intestines and esophagus). Chronic gastritis can also be more serious than ulcers and sometimes lead to complications like anemia or even stomach cancer.
The good news is gastritis often can be treated and even reversed through healthy lifestyle changes, beginning with your diet. Let’s take a look at how your diet influences gastritis along with how the gastritis diet treatment plan can help treat this uncomfortable, potentially dangerous condition.
How Your Diet Contributes to Gastritis
Adjusting your diet is one important step in helping the stomach lining heal and preventing inflammation from developing in the first place — or from returning. That’s why you want to follow a gastritis diet treatment plan if you have this condition. Acute gastritis and stomach ulcer symptoms usually go away within several weeks when someone removes the irritants that cause stomach inflammation and erosion to develop. Studies suggest that other steps to reduce gastritis and stomach ulcers include limiting or eliminating use of nonsteroidal anti-inflammatory drugs (NSAIDs), quitting smoking, lowering alcohol consumption, reducing stress, and improving immune function. (1)
Certain foods can make gastritis symptoms worse and should be avoided on a gastritis diet to help control symptoms while you heal. These include very acidic foods, spicy or hot foods, alcohol , caffeine, and processed/packaged foods. (2) On the other hand, foods high in fiber, antioxidants like vitamin C, electrolytes like magnesium and calcium, vitamin B12, probiotics and omega-3 fatty acids can help lower inflammation and boost digestive health.
A healing gastritis diet that features mostly vegetables, fruits, high-quality proteins and healthy fats can help manage painful symptoms, allow you to maintain a healthy weight, and prevent deficiencies in critical vitamins, minerals and antioxidants that can lead to further complications down the road.
Facts About Gastritis:
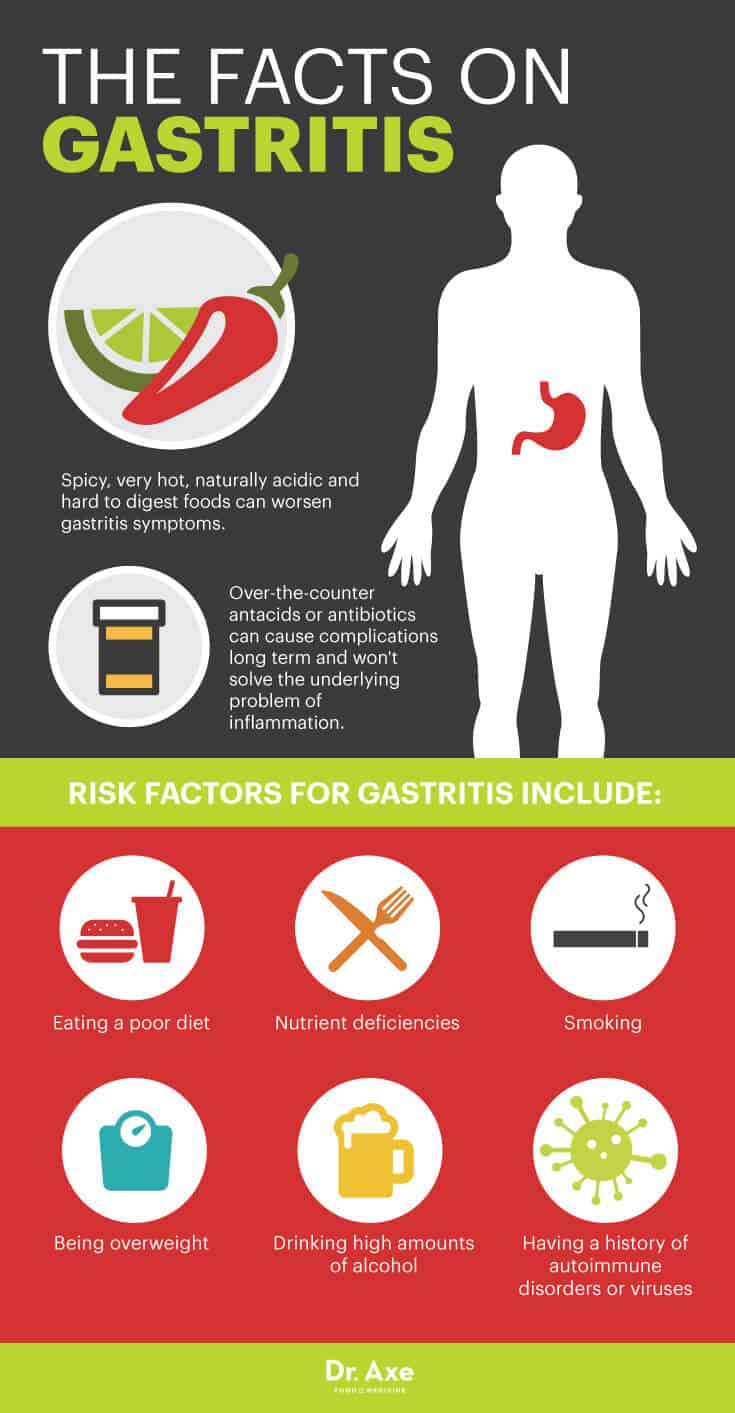
- Many people report worsened gastritis and stomach ulcer symptoms when consuming foods that are spicy, very hot, naturally acidic (like tomatoes and oranges, for example) and hard to digest because they promote inflammation or the release of stomach acids.
- Risk factors for gastritis include eating a poor diet, nutrient deficiencies, smoking, being overweight, drinking high amounts of alcohol, and having a history of autoimmune disorders or viruses. (3)
- While it’s common for people with gastritis or ulcers to rely on taking over-the-counter antacids or antibiotics to treat symptoms, these can cause complications long term (like changes in electrolyte levels, constipation and diarrhea) and don’t solve the underlying problem of inflammation.
Gastritis Diet Plan & Natural Treatments
Each person with gastritis or peptic ulcers reacts differently to various foods, so it’s best to try an elimination diet to kick-start your gastritis diet in order to test which foods tend to cause you the worst pain or help provide relief. First try eliminating all of the common trigger foods described below for a period of time, such as several weeks, and then you can add back one food at a time to test its effects.
By gradually introducing only one or two trigger foods into your diet you will be able to tell if they should be avoided long term or not to control your symptoms.
To get the most benefits from following a gastritis diet plan, use these tips to help manage symptoms:
- Eat smaller meals: Instead of eating fewer meals per day, with larger quantities of food at each meal, try eating smaller amounts more frequently. For example, rather than having three meals daily, plan to have five to six smaller meals every few hours. Eating smaller amounts more often can help increase blood flow to the stomach, which boosts healing — plus food in manageable portions can help buffer the effects of acid lurking in the stomach. (4)
- Avoid eating too close to bedtime: Give yourself about three to four hours before going to sleep to fully digest.
- Drink enough water: Water (but not other liquids like coffee, tea, alcohol or sweetened drinks) seems to help control gastritis symptoms, so aim for at least six to eight glasses daily. Try having a full glass of water when symptoms come up and a glass with every meal. Unlike milk, alcohol and caffeine, water won’t increase stomach acid production or cause burning.
- Reduce stress: Emotional stress alone is no longer believed to be the culprit for stomach erosion, gastritis or ulcers, but it certainly worsens symptoms. Stress can trigger an increased release of stomach acid and raise inflammation — plus it lowers immune function and contributes to other digestive issues. Utilize natural stress relievers to help promote healing in conjuction with following a gastritis diet.
- Quit smoking and lower toxin exposure: Smoking and living an unhealthy lifestyle are major risk factors for developing stomach damage and gastritis. Smoking slows the healing of gastric mucosa, raises the reoccurence rate of ulcers and also makes it more likely you’ll develop infections.
- Take beneficial supplements: Supplements that can help you heal from gastritis include omega-3 fatty acids, probiotics, vitamin C, adaptogen herbs, vitamin B12 and a daily food-based multivitamin.
To help stop gastritis pain and lower your risk for reoccurrence, here are the foods that experts advise you avoid and consume on the gastritis diet treatment plan:
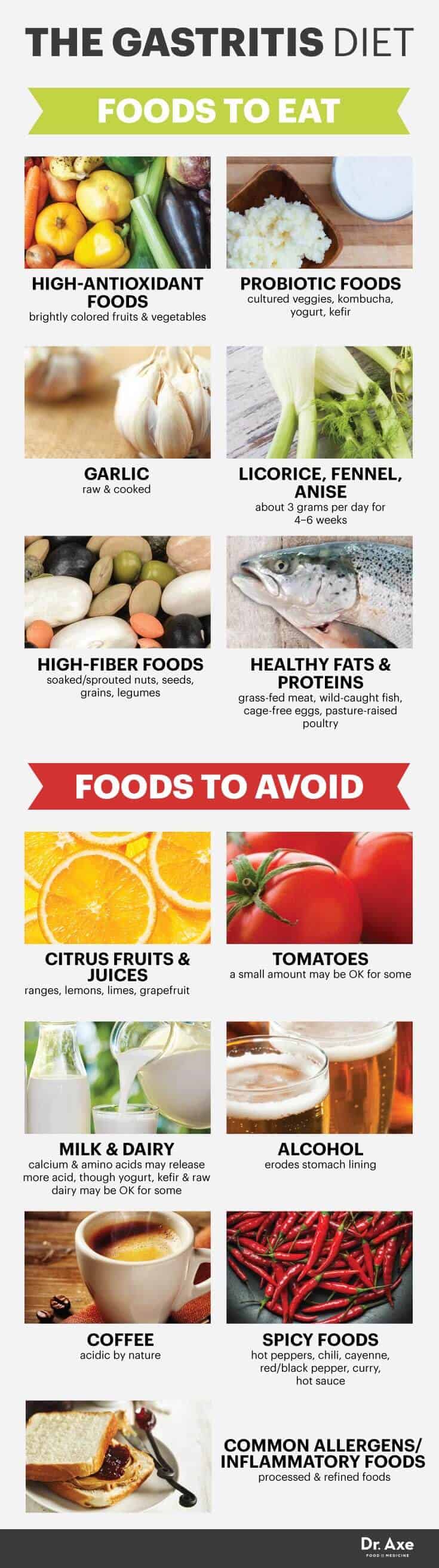
Foods to Avoid that Worsen Gastritis
- Citrus fruits and juices: Citrus fruits, including oranges, lemons, limes and grapefruit, are high in natural acids that can normally be beneficial — however, for people with ulcers or gastritis they’re capable of causing pain. Research suggests that citrus fruits trigger the release of pain-causing chemical neurotransmitters in people with inflammation of the stomach.
- Tomatoes: Tomatoes are similar to citrus fruits in that they’re acidic and can irritate a sensitive stomach. A small amount might be OK for some people, but others feel best avoiding tomato products all together.
- Milk and other dairy products: For years, doctors used to tell gastritis and ulcer patients to drink milk in order to coat the stomach and help block the effects of acids — however, this advice is no longer believed to be helpful. Experts now believe that milk’s calcium and amino acids (proteins) actually stimulate the release of more acid production and can make gastritis symptoms worse. Test your personal reaction to dairy products, including yogurt, kefir, raw cheese and raw milk. If they don’t cause an increase in symptoms, then you can choose to keep consuming these foods, since otherwise they have many benefits to offer. For example, fermented probiotic yogurt has been shown to actually help soothe stomach irritation and reduce GI troubles since it’s a great source of probiotics. (5)
- Alcohol: Alcohol in excess can erode the stomach lining and make inflammation worse. Some people don’t notice an increase in gastritis symptoms when they drink moderately (about one drink per day or less), but others can’t consume alcohol at all without triggering symptoms. Alcohol doesn’t necessarily have to be eliminated all together in most cases; in fact, studies show moderate consumption might even offer protection against gastritis. (6)
- Coffee: Coffee won’t cause stomach troubles or ulcers in most cases, but it usually makes gastritis symptoms worse. In some instances, even when coffee is decaffeinated, it can still trigger pain. Coffee is acidic by nature and might increase feelings of burning — plus caffeine can worsen GI trouble in general for some people. However, several studies show that regular green tea consumption is associated with a 40 percent lower risk for gastritis because it’s anti-inflammatory and much lower in caffeine, helping you avoid caffeine overdose while helping heal the gut.
- Spicy foods: Spicy or hot foods won’t cause gastritis or ulcers, but they can worsen symptoms. These include hot peppers, chili, cayenne, red/black pepper, curry and hot sauce, all of which can cause exacerbation of gastritis symptoms. (7)
- Common allergens and inflammatory foods: Avoid refined and processed foods, such as white breads, pastas, products with added sugar, factory-farm meat, trans fats, refined vegetable oils, fried foods and pasteurized dairy products. These can all trigger food allergies, raise inflammation in the gut, slow healing and make you more prone to infection.
Foods to Consume that Help You Overcome Gastritis
- High-antioxidant foods: Research shows that high-antioxidant foods, such as those high in vitamin C, vitamin A and flavonoids (found in berries, for example), can help lower stomach inflammation and reduce risk for digestive disorders or complications. The best sources of healing antioxidants are brightly colored fresh fruits and vegetables. According to sources such as the University of Maryland Medical Center, fresh fruits, herbs/spices and veggies that are especially beneficial for gastritis include onions, garlic, squash, bell peppers, leafy greens, artichoke, asparagus, celery, fennel, sea vegetables, ginger, turmeric, cruciferous veggies, berries, apples and cranberries. (8)
- Probiotic foods: A review of studies suggests that consumption of probiotics can help control H. pylori bacteria and treat infections of the GI tract that trigger gastritis and ulcers. (9) Probiotic foods, including cultured veggies, kombucha, yogurt and kefir (if you can tolerate dairy), have numerous benefits for almost every aspect of health. They reduce inflammation, regulate bowel movements, help control reactions to food allergies or intolerances, and much more. Probiotic foods and supplements that contain beneficial bacteria such as Lactobacillus bulgaricus might be able to help regulate how much acid the stomach produces and reduce inflammation by significantly inhibiting the expression of cytokines and chemokines.
- Garlic: Consuming both raw and cooked garlic has been a natural remedy for GI troubles for thousands of years. Garlic is a natural anti-inflammatory and even has some antibiotic properties. Some experts believe that raw garlic might even be able to help reduce H. pylori bacteria and inhibit the growth of other harmful bacteria in the microbiome. (10) One study done by the National Cancer Center Research Institute in Tokyo found that when garlic extract was fed to animals at doses of 1 percent, 2 percent and 4 percent, the higher the dose administered the stronger the effects were. H. pylori-induced gastritis in the animals was decreased in a dose-dependent manner significantly over the course of six weeks. Other studies suggest that consuming about two cloves of garlic per day offers the most protection against stomach inflammation, although less is beneficial too, as is taking concentrated garlic extract supplements.
- Licorice, fennel or anise: Licorice is a traditional folk remedy for all sorts of digestive complaints, including ulcers and acid reflux. Licorice root contains a special compound called glycyrrhizic, which is known for its soothing effects on the stomach and strengthening abilities within the GI tract. In fact, this compound is so impressive it’s been shown to have “anti-inflammatory, anti-diabetic, antioxidant, anti-tumor, antimicrobial and anti-viral properties.” (11) While licorice extract might be most beneficial, eating fennel and using anise spices can also offer some relief. Dosage recommendations of licorice extract differs from person to person, but most people are able to experience some improvements taking about three grams per day for about four to six weeks. However, talk to your doctor if you take any prescriptions that can interact with licorice exact, such as those used to treat high blood pressure.
- Foods high in fiber (soaked/sprouted nuts, seeds, grains and legumes): A diet high in fiber has been shown to be beneficial for gastritis and other digestive disorders. A study done by the Harvard School of Public Health found that high-fiber diets were associated with reduced risk for developing stomach ulcers by up to 60 percent. (12) Some of the best sources of fiber include nuts like almonds, seeds like chia or flax, soaked legumes/beans, and sprouted whole grains (preferably those that are ancient grains and gluten-free like oats, quinoa, wild rice, buckwheat and amaranth).
- Healthy fats and proteins: Lean proteins help repair the gut wall and treat digestive issues like leaky gut syndrome, which can trigger inflammation. Good sources of clean protein include grass-fed meat, wild-caught fish, cage-free eggs or pasture-raised poultry. Fish such as salmon or sardines are especially beneficial because they are omega-3 foods that are anti-inflammatory and beneficial for gastritis sufferers. Other healthy fats that are easy to digest include coconut or olive oil, avocado, grass-fed butter and ghee.
The Causes & Symptoms of Gastritis
The most common symptoms of gastritis include: (13)
- burning sensations in or above the stomach/abdomen, especially around the time of eating
- stomachaches or pains
- nausea or vomiting
- loss of appetite, feeling very full quickly and possibly experiencing changes in weight
- hiccups and burping
- changes in bowel movements and the appearance of stools (poop might be darker than usual and take on a tar-like or bloody color)
What causes gastritis to develop?
Gastritis is triggered by inflammation of the stomach and erosion of the stomach’s protective lining. Digestion of the foods you eat first begins in your mouth, before partially digested foods makes their way to your stomach, where they’re coated with acids and enzymes. Every time you eat something your stomach pumps out acids that are actually strong enough to cause damage to the lining of your GI tract — however, normally these acids are buffered by a special type of mucous that blocks the acids’ effects.
Sponge-like mucous coats and protects the lining of the stomach and builds a defense against the painful effects of acids, so when mucous production is decreased for some reason, burning sensations and stomach ulcers in the digestive system are usually experienced. There are a number of different underlying reasons that inflammation develops in the stomach and mucous production is altered.
Risk factors for gastritis include:
- Older age, especially being over 60
- Having low immune function
- Infections caused by the bacteria Helicobacter pylori (H. pylori)
- The overuse of NSAIDs and painkillers, including ibuprofen overdose and aspirin reliance
- A poor diet and nutrient deficiencies (including being deficient in vitamin B12 or low in magnesium, calcium, zinc and selenium)
- Consuming excessive alcohol or smoking cigarettes
- High levels of stress
- Other health conditions that affect the digestive system, including bile reflux, Crohn’s disease or ulcerative colitis, allergies, thyroid disorder, an autoimmune disorder, or viruses like HIV/Herpes
- Pernicious anemia, which affects the lining of the stomach and hinders normal absorption of vitamin B12
- Obesity or being overweight can also make symptoms worse
Final Thoughts on the Gastritis Diet
Gastritis is a digestive condition caused by damage and inflammation to gastric mucosa, the lining of the stomach and gastrointestinal tract. Erosion of the stomach lining leads to acid causing burning sensations and pain in the digestive system — and sometimes malabsorption of nutrients.
Certain foods can make gastritis symptoms worse and should be avoided to help control symptoms while you heal. These include very acidic foods, spicy or hot foods, alcohol , caffeine, and processed/packaged foods, and these foods are the ones you want to avoid on a gastritis diet. On the other hand, foods high in fiber, antioxidants like vitamin C, electrolytes like magnesium and calcium, vitamin B12, probiotics and omega-3 fatty acids can help lower inflammation and boost digestive health, which is why they should be included in a gastritis diet treatment plan.
A healing gastritis diet that features mostly vegetables, fruits, high-quality proteins and healthy fats can help manage painful symptoms, allow you to maintain a healthy weight, and prevent deficiencies in critical vitamins, minerals and antioxidants that can lead to further complications down the road.
Each person with gastritis or peptic ulcers reacts differently to various foods, so it’s best to try an elimination diet to test which foods tend to cause you the worst pain or help provide relief. First try eliminating all of the common trigger foods described below for a period of time, such as several weeks, and then you can add back one food at a time to test its effects.
Some more tips when following a gastritis diet include eating smaller meals, avoiding eating too close to bedtime, drinking enough water, reducing stress, quitting smoking, lowering toxin exposure and taking beneficial supplements.
From the sound of it, you might think leaky gut only affects the digestive system, but in reality it can affect more. Because Leaky Gut is so common, and such an enigma, I’m offering a free webinar on all things leaky gut. Click here to learn more about the webinar.

Original article and pictures take draxe.com site

Комментарии
Отправить комментарий